Dental Sutures: Your Complete Guide to Healing After Oral Surgery
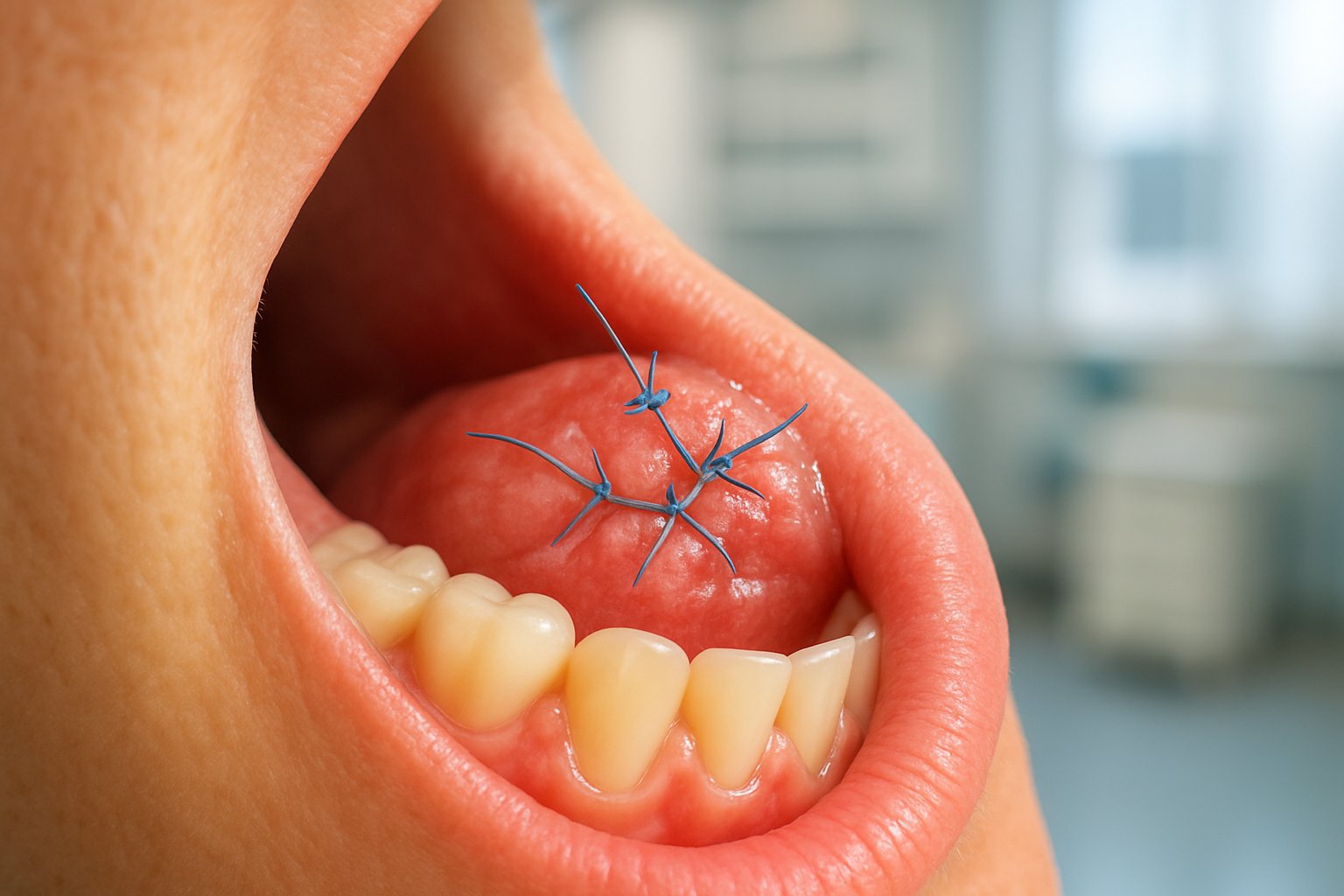
When patients undergo dental surgery, one of the most common concerns involves the small threads used to close wounds and promote healing. These dental sutures play a crucial role in ensuring proper recovery after procedures like tooth extractions, gum surgery, and dental implant placement. Many patients worry about the discomfort, appearance, and care required for these stitches.

Dental sutures are specialized medical threads that help close surgical sites, control bleeding, and support tissue healing while minimizing scarring and complications. Modern dentistry offers various types of sutures, including those that dissolve on their own and others that require removal. The choice depends on the specific procedure, healing requirements, and patient needs.
Understanding what to expect with dental sutures can significantly reduce anxiety and help patients prepare for their recovery journey. From the initial placement through the healing process, knowing how these medical threads work empowers patients to take better care of their oral health and achieve optimal surgical outcomes.
Key Takeaways
- Dental sutures are essential medical threads that close surgical wounds and promote proper healing after dental procedures
- Different types of dental sutures include absorbable varieties that dissolve naturally and non-absorbable ones requiring professional removal
- Proper suture care and following post-operative instructions significantly improve healing outcomes and reduce complications
What Are Dental Sutures?

Dental sutures are specialized medical stitches used to close wounds and incisions in the mouth after oral surgical procedures. They serve multiple functions including wound closure, tissue stabilization, and promoting optimal healing conditions for patients recovering from various dental treatments.
Purpose of Sutures in Dentistry
Dental sutures serve as stitches to close incisions or wounds inside the mouth following various surgical procedures. Their primary function involves bringing tissue edges together to create an environment conducive to proper healing.
Key Functions of Dental Sutures:
- Wound closure – Securely joining separated tissue edges
- Bleeding control – Reducing post-operative bleeding risks
- Infection prevention – Creating a barrier against bacteria
- Tissue support – Maintaining proper positioning during healing
The selection of appropriate suture materials significantly impacts patient outcomes. Choosing optimal dental sutures types can influence recovery speed and overall comfort levels during the healing process.
Sutures also provide mechanical support to weakened tissue areas. This support proves especially important when dealing with delicate gum tissue that requires stable positioning to heal correctly.
How Dental Sutures Aid Healing
Sutures promote healing while helping minimize bleeding and infection through several biological mechanisms. They create optimal conditions for the body’s natural healing processes to occur efficiently.
The healing process begins when sutures hold tissue edges in close approximation. This positioning allows blood vessels to reconnect and new tissue formation to proceed without gaps or disruptions.
Healing Benefits Include:
- Faster tissue regeneration
- Reduced scar formation
- Improved blood flow restoration
- Enhanced cellular migration
Sutures maintain consistent pressure on wound edges, preventing separation during normal mouth movements. This stability proves crucial since the oral environment presents unique challenges with constant moisture and movement from speaking and eating.
The materials used in dental suturing also influence healing rates. Some dissolve naturally over time, eliminating the need for removal appointments while supporting tissue throughout critical healing phases.
Common Procedures Requiring Sutures
Multiple dental and oral surgery procedures routinely require sutures to ensure proper healing outcomes. Tooth extractions represent one of the most frequent applications, particularly for complex removals involving surgical access.
Procedures Commonly Using Sutures:
- Wisdom tooth removal – Complex extractions requiring tissue closure
- Dental implant placements – Securing gum tissue over implant sites
- Gum surgery – Periodontal procedures and tissue grafts
- Oral biopsies – Closing small incision sites
Implant placements often require sutures to protect the surgical site during the critical integration period. The sutures maintain proper gum tissue positioning while the implant bonds with surrounding bone.
Periodontal surgery frequently involves suturing to reposition gum tissue or secure grafted materials. These procedures rely on precise suture placement to achieve desired aesthetic and functional results.
Emergency dental procedures may also require immediate suturing to control bleeding and protect exposed areas until definitive treatment can be completed.
Types of Dental Sutures

Dental professionals categorize sutures into two main groups: those that dissolve naturally in the mouth and those that require removal after healing. The choice between synthetic and natural materials further influences healing outcomes and patient comfort.
Absorbable Sutures
Absorbable sutures dissolve naturally in the oral environment without requiring removal appointments. These sutures break down through the body’s natural processes over time.
Polyglycolic Acid (PGA) sutures offer excellent strength and predictable absorption rates. They typically dissolve within 7-14 days, making them ideal for routine extractions and minor oral surgeries.
Polylactic Acid (PLA) provides longer-lasting support with absorption occurring over 2-4 weeks. Dental surgeons often choose PLA for procedures requiring extended tissue support during healing.
Vicryl represents a popular synthetic option that combines reliability with patient comfort. It maintains tensile strength for approximately one week before beginning the absorption process.
Chromic gut sutures come from natural collagen but undergo chemical treatment to slow absorption. Traditional gut sutures absorb faster than chromic varieties, typically within 3-7 days.
Patients appreciate absorbable options because they eliminate follow-up removal appointments. These sutures work particularly well in areas where access is limited and patients may struggle to return for follow-up care.
Non-Absorbable Sutures
Non-absorbable sutures require scheduled removal by dental professionals after tissue healing occurs. These materials maintain their strength and structure indefinitely in the oral environment.
Silk sutures provide excellent handling characteristics and patient comfort during placement. Dentists can tie silk easily and patients rarely experience irritation from the soft material.
Nylon offers superior strength and minimal tissue reaction. The synthetic material resists bacterial adherence better than natural alternatives, reducing infection risks.
Polypropylene delivers exceptional durability with the least tissue reaction among non-absorbable options. Its smooth surface allows for easy removal while minimizing patient discomfort.
Dental professionals typically remove non-absorbable sutures within 7-14 days after surgery. The selection of appropriate suture material can greatly influence surgical outcomes and patient recovery experiences.
Non-absorbable sutures work best for procedures requiring precise wound edge alignment. They provide consistent tension and support throughout the critical healing period.
Synthetic vs. Natural Suture Materials
Synthetic suture materials offer predictable performance and consistent quality control. Manufacturing processes ensure uniform diameter, strength, and absorption rates across batches.
Modern synthetic options like PGA and PLA provide superior biocompatibility compared to older materials. They produce minimal inflammatory responses and integrate well with healing tissues.
Natural suture materials include traditional gut sutures derived from animal collagen. These materials absorb through enzymatic processes that can vary between patients.
| Material Type | Absorption Time | Strength Retention | Tissue Reaction |
|---|---|---|---|
| Synthetic PGA | 7-14 days | Excellent | Minimal |
| Chromic Gut | 10-21 days | Moderate | Moderate |
| Silk | Non-absorbable | Excellent | Low |
| Nylon | Non-absorbable | Superior | Minimal |
Synthetic materials generally provide more predictable healing outcomes. Their consistent properties allow dental surgeons to anticipate exactly how tissues will respond during recovery.
Natural materials may cause slightly more tissue inflammation as they break down. However, some patients prefer knowing their sutures come from biological sources rather than manufactured polymers.
Suture Selection and Placement in Dentistry
The choice of suture material and proper placement technique directly impacts healing success, patient comfort, and surgical outcomes. Key considerations include material properties, anatomical location, and the specific requirements of each dental procedure.
Factors Influencing Suture Choice
Several critical factors guide dentists when selecting appropriate suture materials for different procedures. The location of the surgical site plays a primary role in material selection.
Monofilament sutures consist of a single strand and glide smoothly through tissues. They resist bacterial accumulation and work well in areas prone to infection. These sutures create less tissue trauma during placement.
Multifilament sutures feature multiple twisted or braided strands. They offer superior handling characteristics and knot security. However, they may harbor bacteria between the fibers in contaminated environments.
The procedure type determines whether absorbable or non-absorbable materials work best. Absorbable sutures dissolve naturally and eliminate the need for removal appointments. Non-absorbable sutures provide longer-lasting support but require removal.
Patient factors influence material choice significantly. Age, healing capacity, and oral hygiene habits affect suture performance. Patients with compromised immune systems may benefit from absorbable materials to reduce infection risk.
Suturing Techniques
Proper suturing techniques ensure optimal tissue stabilization and promote predictable healing outcomes. The interrupted suture technique places individual stitches with separate knots for each suture.
This method allows selective suture removal if complications arise. Each stitch functions independently, so failure of one suture doesn’t compromise the entire closure.
Continuous suturing uses a single strand to close the entire wound length. This technique provides uniform tension distribution and faster placement. It works particularly well for long incisions requiring consistent closure.
Mattress sutures penetrate deeper tissue layers and provide enhanced wound edge approximation. Horizontal mattress sutures distribute tension over broader tissue areas. Vertical mattress sutures help evert wound edges for optimal healing.
The surgeon’s needle selection affects placement success. Curved needles navigate oral anatomy more easily than straight needles. The needle size should match the suture material thickness for optimal performance.
Knot Security and Tensile Strength
Tensile strength determines how much force sutures can withstand before breaking during the healing process. This property varies significantly between different suture materials and affects clinical performance.
Knot security prevents suture loosening under normal oral function stresses. Proper knot tying technique requires specific throw sequences for different materials. Monofilament sutures typically need additional throws to maintain knot integrity.
Hemostasis depends partly on appropriate suture tension and placement. Overtightening sutures can compromise blood supply and delay healing. Undertightening fails to control bleeding and may allow wound separation.
The surgeon must balance adequate closure tension with tissue viability. Excessive tension causes tissue blanching and potential necrosis. Proper placement achieves wound approximation without compromising circulation.
Different materials lose tensile strength at varying rates during healing. Some retain strength for weeks, while others weaken within days. The expected healing timeline influences material selection for specific procedures.
Patient Experience and Recovery
The patient’s journey with dental sutures involves three critical phases that directly impact comfort and healing success. Recovery time varies based on suture material choice, while tissue compatibility affects daily comfort levels, and removal procedures influence overall treatment convenience.
Healing Time with Dental Sutures
Absorbable sutures typically dissolve within 7-14 days, eliminating the need for removal appointments. These materials break down naturally as tissues heal, making them ideal for patients who prefer minimal follow-up visits.
Non-absorbable sutures require removal after 5-10 days depending on the surgical site. The healing timeline follows a predictable pattern during this period.
Patients experience initial discomfort for the first 24-48 hours. Swelling peaks around day 2-3, then gradually subsides. Most patients report significant improvement by day 5.
Factors affecting healing time include:
- Patient age and overall health
- Surgical complexity
- Oral hygiene compliance
- Smoking status
Recovery time after dental surgery can range from 7 to 15 days, depending on the procedure type and individual healing capacity.
Tissue Reactivity and Patient Comfort
Silk sutures may cause mild inflammatory responses in sensitive patients. Some individuals experience localized redness or slight irritation around suture sites. This reaction typically resolves within 2-3 days.
Synthetic materials like nylon and polypropylene demonstrate excellent biocompatibility. These sutures rarely trigger adverse tissue reactions, making them suitable for patients with sensitive oral tissues.
Absorbable options such as Vicryl and PDS cause minimal tissue reactivity. As these materials break down, they release byproducts that tissues tolerate well.
Patients with known allergies should discuss material options beforehand. Signs of problematic tissue reactivity include:
- Persistent swelling beyond day 4
- Unusual redness or warmth
- Increased pain after initial improvement
Most patients tolerate all suture types well when proper care and attention to post-procedure healing guidelines are followed.
Suture Removal and Patient Convenience
Absorbable sutures offer maximum patient convenience by eliminating removal appointments. Patients appreciate not scheduling additional visits during their recovery period. These sutures dissolve gradually without patient intervention.
Non-absorbable suture removal takes 2-5 minutes per appointment. The process involves minimal discomfort, often described as slight tugging or pinching sensations.
Removal procedure steps:
- Gentle cleaning of the suture area
- Cutting one side of each suture
- Careful extraction of suture material
- Brief examination of healing progress
Some patients prefer non-absorbable options despite requiring removal. They value the predictable timeline and the opportunity for professional healing assessment.
Timing considerations affect patient scheduling convenience. Morning appointments often work better as patients experience less sensitivity earlier in the day.
The choice between suture types balances healing requirements with patient lifestyle preferences and appointment availability.
Applications and Outcomes of Dental Sutures
Dental sutures serve critical functions across various oral surgical procedures, from routine periodontal treatments to complex implant placements. The proper selection and application of sutures directly impacts healing success, patient comfort, and long-term treatment outcomes.
Periodontal Surgeries and Gum Grafting
Periodontal surgeries rely heavily on precise suturing techniques to ensure proper tissue healing and gum attachment. During gum disease treatment, dentists use sutures to secure tissue flaps after deep cleaning procedures or bone grafting.
Soft tissue grafting represents one of the most suture-dependent procedures in dentistry. Patients receiving gum grafts to cover exposed tooth roots require meticulous suturing to hold the new tissue in place. The donor tissue must remain stable during the critical first week of healing.
Surgeons typically choose absorbable sutures for periodontal work because they eliminate the need for removal appointments. These sutures dissolve naturally as the gums heal, reducing patient visits and discomfort.
Key periodontal suturing applications include:
- Flap surgery for deep pocket treatment
- Connective tissue grafts for root coverage
- Regenerative procedures with bone grafts
- Crown lengthening surgeries
Success rates for periodontal procedures improve significantly when appropriate suturing materials match the specific tissue requirements and healing timeline.
Implant Procedures and Oral Surgery
Implant procedures demand specialized suturing approaches due to the precision required for optimal healing around titanium fixtures. Surgeons must ensure complete tissue coverage over the implant site while maintaining adequate blood supply to the area.
Primary closure techniques using non-absorbable sutures often provide the most predictable results for implant placement. These sutures allow for controlled healing and can be removed once initial tissue integration occurs.
Oral surgery applications extend beyond implants to include wisdom tooth extractions, cyst removals, and corrective jaw procedures. Each surgery type requires specific suturing considerations based on tissue thickness, tension levels, and expected healing patterns.
Complex extractions, particularly impacted wisdom teeth, benefit from careful suturing to prevent dry socket formation. The sutures help maintain blood clot stability and reduce post-operative complications.
Common oral surgery suturing needs:
- Socket preservation after extractions
- Sinus lift procedures
- Bone augmentation surgeries
- Soft tissue management around implants
Surgical Outcomes and Preventive Care
Surgical outcomes improve dramatically when patients receive proper suturing combined with clear post-operative instructions. Studies show that appropriate suture selection can greatly influence surgical outcomes and patient recovery.
Infection prevention relies partially on suturing technique quality. Well-placed sutures create barriers against bacterial invasion while promoting natural healing processes. Patients experience less swelling and discomfort when tissues receive adequate support through proper suturing.
Preventive care aspects include teaching patients how to maintain oral hygiene around sutures without disturbing healing tissues. Gentle brushing techniques and prescribed mouth rinses help prevent complications during the recovery period.
Healing timelines vary based on suture type and surgical complexity. Absorbable sutures typically dissolve within 7-14 days, while non-absorbable options require removal appointments after 5-10 days.
Factors affecting suture success:
- Patient compliance with post-operative care
- Suture material biocompatibility
- Surgical site cleanliness
- Individual healing capacity
- Proper tension distribution
Regular follow-up appointments allow dentists to monitor suture integrity and address any concerns before complications develop.
Frequently Asked Questions
Patients often have concerns about dental sutures, from understanding the different materials used to knowing what to expect during healing. These common questions address everything from suture types and placement techniques to costs and removal procedures.
What are the different types of sutures used in dental procedures?
Dental professionals use two main categories of sutures: absorbable and non-absorbable materials. Absorbable sutures dissolve naturally over time, eliminating the need for a separate removal appointment.
Common absorbable options include chromic gut, which dissolves in 7-10 days, and synthetic materials like polyglactin that break down over 2-3 weeks. These work well for routine extractions and minor oral surgeries.
Non-absorbable sutures like silk, nylon, or polypropylene require manual removal but offer stronger wound closure. Dentists often choose these for more complex procedures or areas that need extended healing support.
The material selection depends on the specific procedure, healing requirements, and the patient’s individual needs. Each type has unique properties that make it suitable for different dental applications.
Can you explain the various techniques for suturing in dental surgeries?
Dental professionals use several suturing techniques during oral surgery depending on the wound type and location. The simple interrupted suture is most common, involving individual stitches placed separately across the wound.
Continuous suturing uses one long thread to close the entire incision, similar to a running stitch. This technique works well for longer incisions and provides even tension distribution.
Mattress sutures involve deeper tissue layers and create stronger wound closure. Horizontal mattress sutures provide excellent eversion of wound edges, while vertical ones offer superior strength.
Figure-eight sutures help control bleeding in extraction sites by applying pressure to surrounding tissues. Surgeons often use this technique after tooth removal to promote clot formation.
The chosen technique depends on factors like wound size, tissue type, and desired healing outcomes. Experienced dental surgeons select the most appropriate method for each unique situation.
How much does it generally cost to get sutures in a dental clinic?
Suture costs are typically included in the overall price of dental procedures rather than charged separately. Simple suturing after extractions usually adds $25-75 to the total treatment cost.
More complex suturing for surgical procedures can range from $100-300 depending on the technique complexity and number of sutures required. Insurance coverage often includes suturing as part of necessary dental treatment.
Geographic location significantly affects pricing, with urban areas generally charging more than rural clinics. The type of suture material used can also influence the final cost.
Patients should ask for detailed treatment estimates that break down all associated costs. Most dental offices provide written estimates that include suturing fees within the procedure pricing.
How do I know which suture sizes are appropriate for my dental treatment?
Dental professionals determine appropriate suture sizes based on the treatment area and tissue thickness. Smaller numbers indicate thicker sutures, while larger numbers represent finer materials.
Common dental suture sizes range from 3-0 (thicker) to 6-0 (very fine). Oral surgeons typically use 3-0 or 4-0 sutures for extraction sites and gum procedures.
Delicate areas like the tongue or inner cheek require finer 5-0 or 6-0 sutures to minimize tissue trauma. Thicker sutures provide stronger closure but may cause more discomfort.
The dentist considers factors like wound tension, healing time, and patient comfort when selecting suture size. Patients don’t need to worry about these technical details as their dental professional handles all sizing decisions.
What is the average time it takes for dental sutures to dissolve on their own?
Absorbable dental sutures typically dissolve within 7-21 days depending on the material used and individual healing rates. Chromic gut sutures usually disappear within the first week.
Synthetic absorbable materials like polyglactin or polydioxanone take 2-3 weeks to fully dissolve. These materials maintain their strength longer, providing extended wound support during healing.
Patients may notice small pieces of suture material coming loose before complete dissolution occurs. This is normal and doesn’t indicate a problem with the healing process.
Individual factors like age, overall health, and oral hygiene can affect dissolution rates. Some patients experience faster breakdown while others may see remnants for slightly longer periods.
What should I expect during the removal of dental sutures?
Non-absorbable suture removal is a quick, minimally uncomfortable procedure typically scheduled 7-14 days after placement. The dentist uses small scissors or a suture removal tool to cut and gently pull out each stitch.
Most patients describe the sensation as slight tugging or pinching rather than pain. The removal process usually takes only a few minutes, even for multiple sutures.
Patients should expect some minor bleeding or sensitivity at the suture sites immediately after removal. This typically resolves within a few hours as the small puncture sites heal.
The dentist will examine the healing progress and provide any additional care instructions during the removal appointment. Proper wound healing should be evident by this time, with tissues appearing pink and well-approximated.